NEW DELHI: India has one of the highest death tolls in the world, but the country still does not know what is killing most people – a gap that is most pronounced in northern India and even the national capital. A nationwide study published in Scientific Reports found that only 22.5% of deaths in India are medically confirmed, leaving nearly four out of five deaths without a medically confirmed cause in the official records. The results are particularly significant for Delhi and the northern Indian states, which together make up a large proportion of the population. North India has the worst medical death record, averaging just 13%, while Delhi’s rate has stagnated at around 57-59% for years – far from universal coverage despite its dense network of hospitals and medical colleges. The consequences go far beyond record keeping. “Without knowing the cause of death, it becomes difficult to estimate disease prevalence at a national or regional level, which in turn impacts health care, particularly in remote areas,” said Dr. Vinay Aggarwal, former national president of the Indian Medical Association. He added that poor death documentation also affects processes such as revising the electoral roll, underscoring the wider administrative implications.
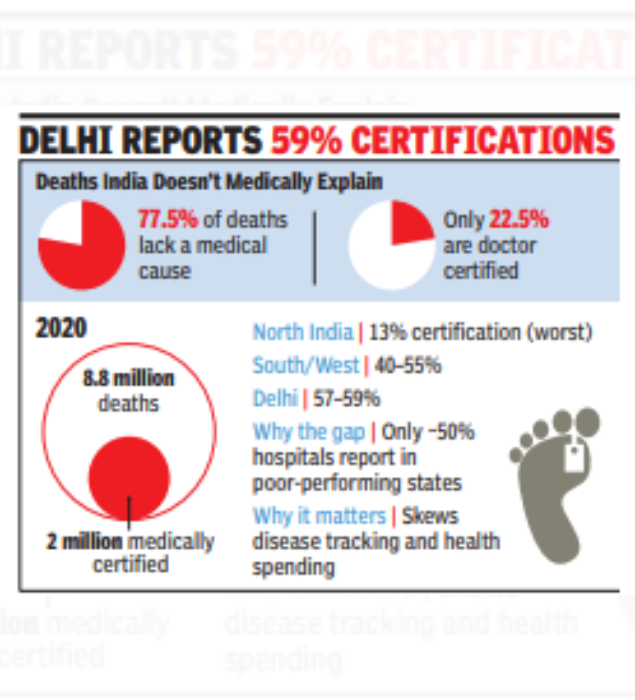
Public health experts warn that unreliable data on causes of death means governments are effectively planning health policies without knowing which diseases are killing people. Deaths from heart disease, stroke, cancer, diabetes, infections, maternal causes, injuries and suicide cannot be accurately recorded, distorting estimates of the burden of disease and skewing health care spending. Weak certification also delays detection of outbreaks and undermines surveillance at a time when noncommunicable diseases account for a growing share of adult deaths. The study tracked death certification patterns across India over a 15-year period, from 2006 to 2020. The regional differences are large. Large parts of northern and eastern India continue to report single-digit or low double-digit certification rates, driving down national averages and leaving millions of deaths without medical explanation each year. In contrast, southern and western states fare far better, reflecting stronger hospital reporting and administrative compliance. Some Union Territories have near-universal coverage – Lakshadweep reports medical certification of over 94%, while Goa has near-complete coverage. The study challenges the assumption that the shortage of doctors alone explains the gap. While poorly performing states have fewer doctors, the strongest factor is whether hospitals actually report deaths. In low-performing states, only about half of registered hospitals report cause of death data, compared to over 90% in high-performing states and UTs. The scale of the problem is enormous. In 2020, India recorded around 8.8 million deaths. While about 80% were registered, only about 2 million had a medically confirmed cause. Progress has been slow, with certification improving by only 2.5 percentage points over a decade despite expanded healthcare infrastructure. Researchers warn that unless medical certificates become routine and enforceable – particularly in northern India and large urban centers like Delhi – India will continue to underestimate major deaths because it knows far more about how many people die than why they die.



